5 Innovative Food Allergy Prevention Strategies

Food allergies affect hundreds of millions of people worldwide, with rising incidence among children and young adults. “Food Allergy Prevent” is a startup set on reducing the risk of sensitization and severe reactions through a prevention-first model that blends evidence-based protocols, at-home testing, and data-driven personalization. This overview explains the problem, the solution stack, and the go-to-market path that can turn prevention into a scalable, trusted service.
The Problem: Rising Incidence and Fragmented Care
Most families navigate food allergies through a maze of self-education, emergency plans, and inconsistent guidance. Traditional care is optimized for diagnosis and reaction management—not prevention. The result is delayed introductions for infants, anxiety around school meals, and high costs from avoidable ER visits. A prevention-first startup addresses three gaps:
- Early risk detection before clinical reactivity develops.
- Standardized introduction protocols tailored to risk level.
- Continuous coaching to maintain tolerance and reduce accidental exposures.
The Prevention Stack: Product + Protocol + Platform
A credible solution mixes clinical rigor with consumer-grade usability.
1) Risk Stratification and Screening
- Family and atopic history intake: eczema, asthma, and prior reactions increase baseline risk.
- Biomarkers and directed testing: total IgE, component-resolved diagnostics (where appropriate), and non-invasive skin/derm history scores to triage who needs specialist referral versus home-based introduction plans.
- Environment mapping: school, daycare, and household food handling practices.
2) Evidence-Based Introduction & Maintenance
- Guided early introduction for infants at appropriate ages (per pediatric guidance) with measured, repeatable dosing schedules.
- Maintenance plans that keep tolerated foods in rotation to prevent loss of tolerance.
- Desensitization hand-offs: for higher-risk profiles, structured referral to allergists for oral immunotherapy (OIT) with data continuity from the app.
Note: The startup should present its protocols as clinician-reviewed and aligned with prevailing pediatric guidance, not as medical replacement.
3) Safety Layer
- Emergency readiness: checklists, epinephrine auto-injector training reminders, school forms, and reaction logging.
- Allergen detection tools: integrations with select third-party detectors and barcode databases; model-based warnings for cross-contamination categories.
- Alerts & thresholds: symptom triage questionnaires that recommend escalation paths (tele-allergy consult → urgent care → ER).
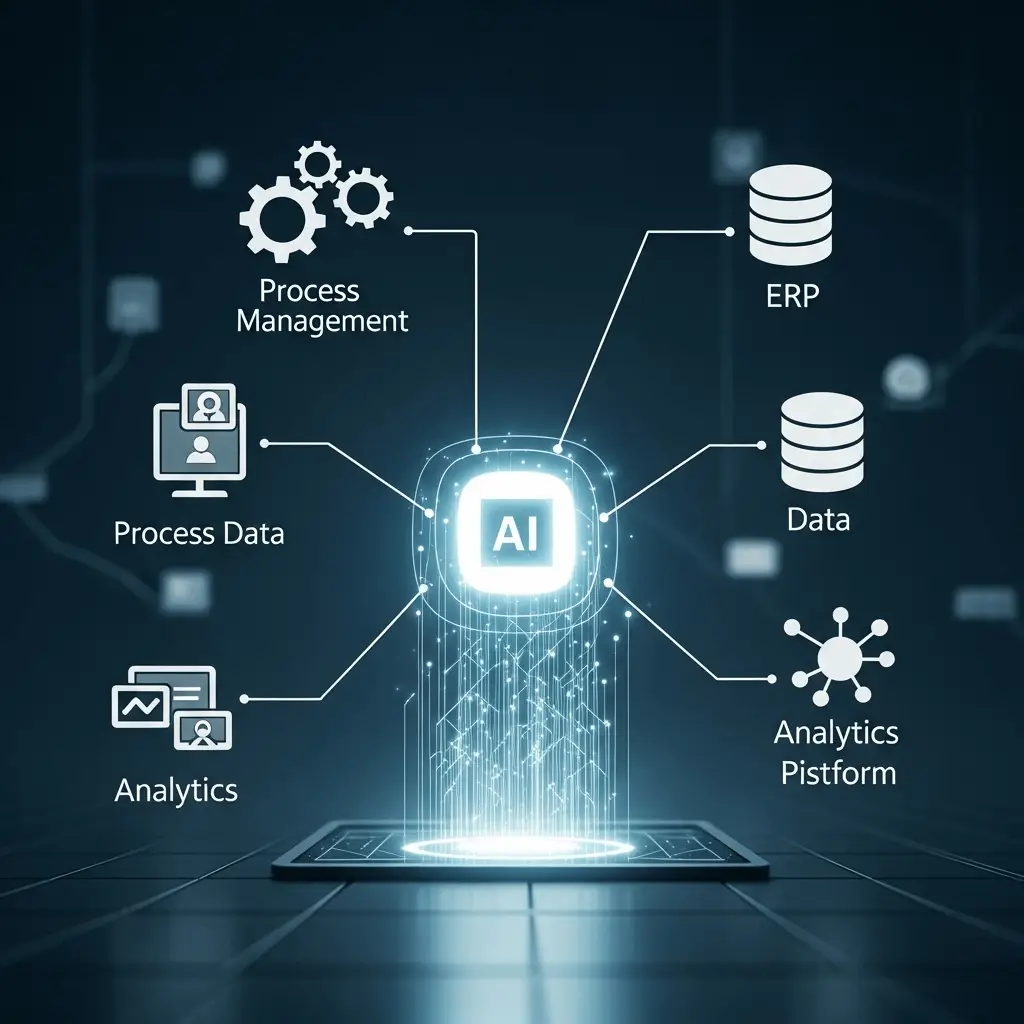
4) Personalization Engine
- Data inputs: age, growth curves, eczema severity, prior exposures, diary of tolerated foods, and reaction history.
- Outputs: staged introduction plans, weekly menus, and micro-doses for maintenance. Suggestions adjust based on adherence, symptoms, and seasonality (e.g., pollen-food syndrome patterns).
The Product: How It Could Work
- Starter Kit: a nurse-reviewed onboarding, lancet-free micro-sample (if clinically justified and permitted), and standardized measuring spoons/snack sachets for home trials in low-risk profiles.
- Mobile App: dosing timers, video walkthroughs, food logs, label scanner, and push alerts. Includes printable school care plans and caregiver instructions.
- Clinician Console: for affiliated allergists/pediatricians to review data, adjust plans, and message families.
- Education Library: short, culturally adapted modules for caregivers, teachers, and food service staff.
Business Model and Pricing
- B2C subscription: monthly plan covering app access, coaching, and kit refills.
- B2B2C partnerships: pediatric groups and health plans that subsidize enrollment for at-risk infants.
- Employer & school programs: prevention bundles and staff training for cafeterias/daycares.
- Add-ons: tele-allergy visits, advanced testing panels, and OIT partner referrals.
Regulatory, Clinical, and Ethical Guardrails
- Regulatory stance: the app is a care-navigation and education tool; any diagnostic claims or in-home testing kits must meet jurisdictional device rules. Clear disclaimers and MD oversight reduce risk.
- Clinical validation: prospective observational cohorts that track introduction success, reaction reduction, and adherence. Publish protocols and outcomes to build trust.
- Data privacy: end-to-end encryption, parental consent flows, de-identified analytics, and transparent data-sharing policies.
- Equity: multilingual content, low-literacy designs, and subsidized plans for low-income families to avoid widening disparities.
Go-to-Market Plan
- Pilot with pediatric clinics in two markets to validate onboarding time, adherence, and safety outcomes.
- KOL advisory board (allergists, dietitians, school nurses) to review content and protocols quarterly.
- Outcomes reporting: publish real-world stats—% successful introductions, reduction in ED visits, caregiver confidence scores.
- Distribution: co-branded kits with hospital networks; employer benefits brokers; partnerships with daycare chains.
- Content and community: webinars, caregiver forums, and meal-planning templates to reduce churn and build word-of-mouth.
Competitive Landscape
- Allergy testing companies: focus on diagnostics; limited prevention coaching.
- Generic nutrition apps: low clinical rigor; no emergency layer.
- Clinic-based OIT programs: strong for desensitization but less scalable for population-level prevention.
“Food Allergy Prevent” differentiates with prevention protocols, remote coaching, and school integration.
Risks and Mitigations
- Adherence drop-off: mitigate via daily nudges, streaks, and quick-win milestones.
- False reassurance: keep strong safety messaging and clear escalation rules.
- Supply chain issues: standardized sachets and local co-packers; maintain SKUs for common allergens and culturally relevant foods.
- Clinical liability: operate under physician oversight, document informed consent, and restrict higher-risk steps to clinic settings.
Key Metrics to Track
- Introduction completion rate per food category.
- Time-to-tolerance and maintenance adherence.
- Reaction incidence per 1,000 dosing events.
- Retention (90/180/365 days) and caregiver confidence surveys.
- School participation and staff training completions.
For more scientific details, visit the Food Allergy Research & Education organization.
You can also read our detailed overview on health innovation here.